When you chew food, the enzymes in your saliva begin the process of digestion.
WHAT
IS EPI?
Exocrine Pancreatic Insufficiency (EPI) is a condition in which your body doesn't provide enough pancreatic enzymes to properly break down food. People with EPI are unable to properly digest the nutrients in food such as fats, proteins, and carbohydrates, leading to maldigestion. Once diagnosed, EPI is a manageable condition when treated with pancreatic enzyme replacement therapy (PERT) as part of an EPI management plan.
What is PERT?
Taken as prescribed, PERT replaces the enzymes your body isn’t providing in order to help you digest food. Once diagnosed with EPI, your doctor or gastroenterologist can prescribe the right dose for you.
To better understand EPI, it helps to know what the pancreas does.
Located in the center of the abdomen, the pancreas has 2 important functions:
- Endocrine function
makes insulin, a hormone that helps the body process the sugar we eat - Exocrine function
makes enzymes to help digest food so the body can absorb it
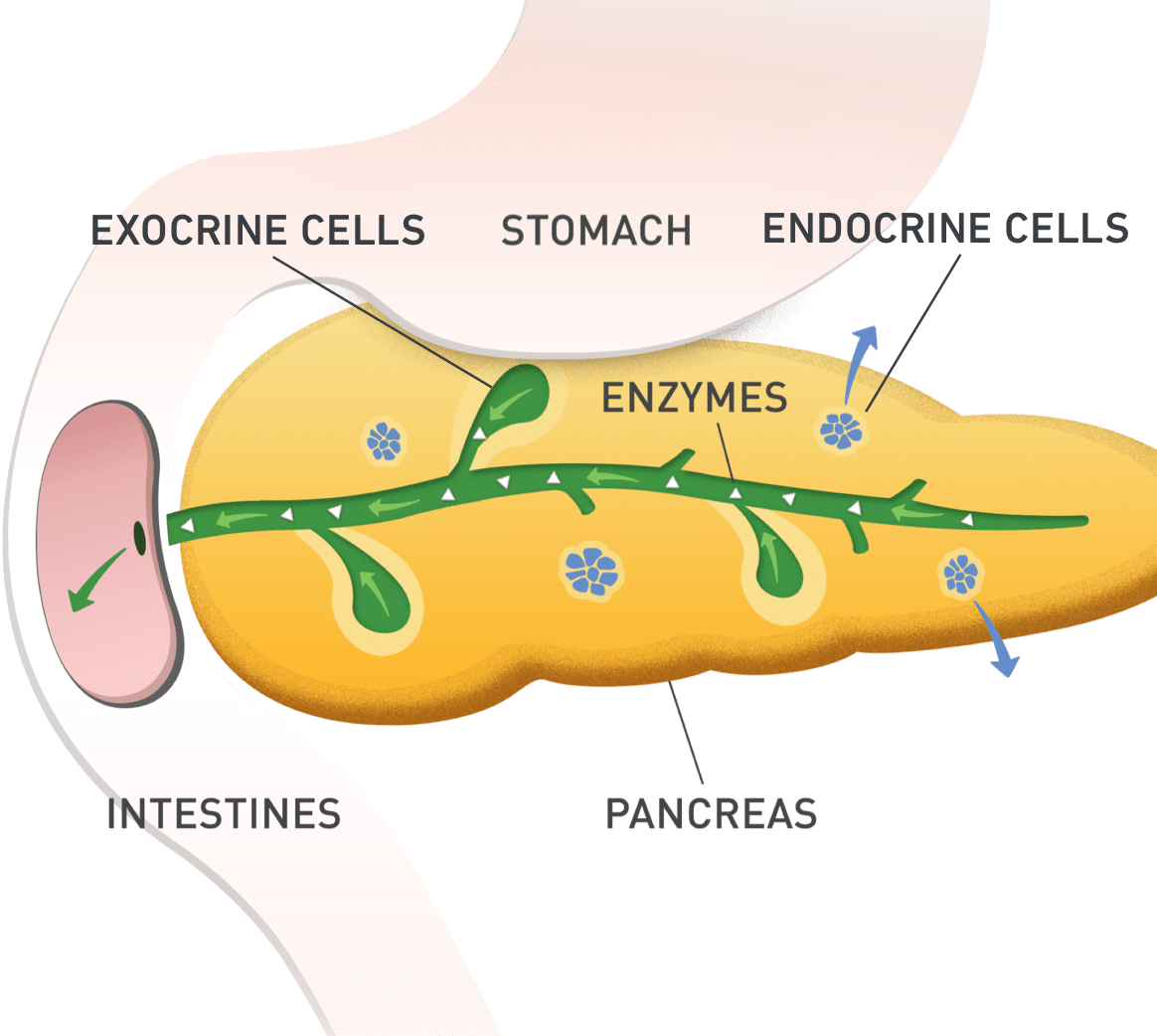
In people with EPI, it’s the exocrine function of the pancreas that is affected. Your body doesn’t produce or supply enough of these pancreatic enzymes needed to break down the food you eat. As a result, EPI affects the way your body digests food, causes unpleasant digestion symptoms, and may prevent you from getting the necessary nutrition from the foods you eat.
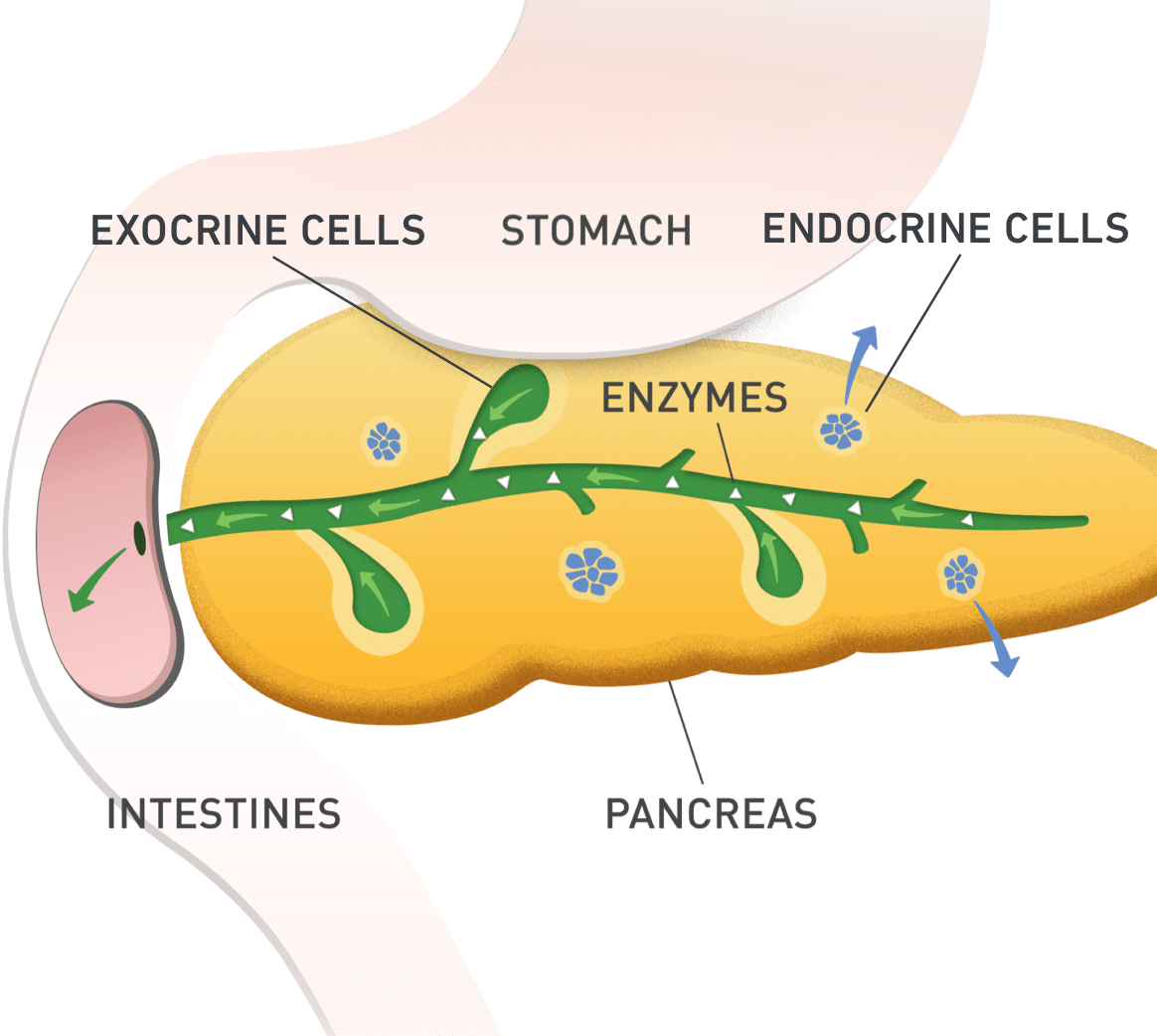
What are the 3 main enzymes produced by the pancreas?
The exocrine function of the pancreas produces 3 main types of enzymes:
Lipase
(breaks down fats)

Protease
(breaks down proteins)

Amylase
(breaks down carbohydrates)


EPI is caused by an underlying condition or procedure. However, the frequency, severity, and variety of EPI symptoms may vary from person to person. It may take months or even years for EPI symptoms to appear. The symptoms of EPI may also be similar to other gastrointestinal disorders, which can make EPI a difficult condition to diagnose.
Only your doctor can determine if EPI is the cause of your symptoms. Use our Symptom Checker to identify your symptoms and help start a discussion with your doctor.
See how EPI affects digestion.
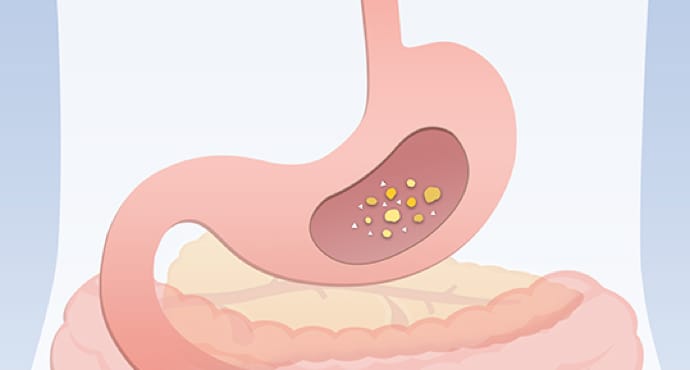
Food mixes with stomach acid and enzymes that further break it down.
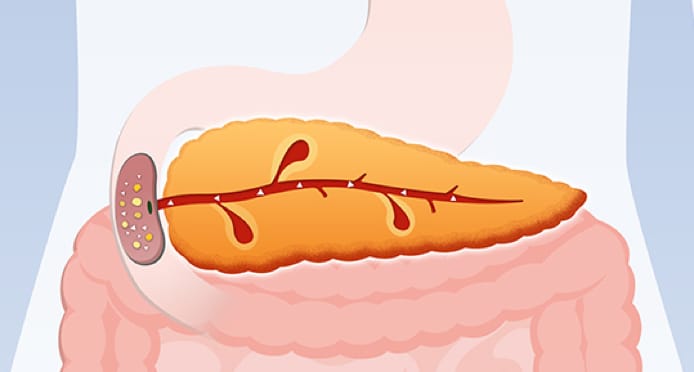
Next, the pancreas releases enzymes that mix with the food as it enters the small intestine. If you have EPI, there is a deficiency of pancreatic enzymes.

With EPI, food doesn’t get broken down the way it should, so your body isn’t able to digest and absorb nutrients properly.
EPI may result in nutrients not being absorbed properly and uncomfortable gastrointestinal symptoms.

Need a doctor experienced in EPI?

How is EPI diagnosed?

How is EPI treated?
Reference sources:
1. Alkaade S, Vareedayah AA. A primer on exocrine pancreatic insufficiency, fat malabsorption, and fatty acid abnormalities. Am J Manag Care. 2017;23(12)(suppl):S203-S209. 2. Singh VK, Haupt ME, Geller DE, Hall JA, Quintana Diez PM. Less common etiologies of exocrine pancreatic insufficiency. World J Gastroenterol. 2017;23(39):7059-7076. 3. Fieker A, Philpott J, Armand M. Enzyme replacement therapy for pancreatic insufficiency: present and future. Clin Exp Gastroenterol. 2011;4:55-73. 4. Pancreatic enzymes. Pancreatic Cancer Action Network website. https://www.pancan.org/facing-pancreatic-cancer/living-with-pancreatic-cancer/diet-and-nutrition/pancreatic-enzymes/. Accessed December 15, 2020. 5. Röder PV, Wu B, Liu Y, Han W. Pancreatic regulation of glucose homeostasis. Exp Mol Med. 2016;48:e219. doi:10.1038/emm.2016.6. 6. Ferrone M, Raimondo M, Scolapio JS. Pancreatic enzyme pharmacotherapy. Pharmacotherapy. 2007;27(6):910-920.

